This activity aims to examine bereavement in nurses following the death of a patient, highlighting the manifestations of grief and consequences of unresolved grief as well as strategies to help nurses cope with grief in a healthy manner to prevent compassion fatigue and promote physical and mental health and well-being.
...purchase below to continue the course
on the concept of working through grief. His work centered on letting go of the bonds and attachment to those who have died, acclimating to a new sphere of normalcy without the deceased, and building new relationships and experiences (DeSpelder et al., 2020; Freud, 1917). In 1969, Elisabeth Kübler-Ross proposed the 'stage 'theory' by publishing her book,
On Death and Dying. This book represented the culmination of hundreds of interviews with dying patients through which she cultivated the theory that there are five stages to death and dying; denial, anger, bargaining, depression, and acceptance (frequently referred to as DABDA). Originally developed to explain the stages patients go through after receiving a terminal or life-limited diagnosis, it was later applied to post-death or post-loss experiences. Kübler-'Ross' model has profoundly impacted the world and is among the most well-known and commonly taught systems for understanding the grieving process. Despite Kübler-Ross stating in the book that the stages can occur in any order and some simultaneously, it received criticism for being a linear model by those that did not understand or read the text thoroughly. The concepts have since been clarified to make clear that the emotional states and adaptive mechanisms associated with the five stages of grief occur in a variety of patterns. Some people will not go through each stage, whereas others may repeat stages. The stages often overlap, as they are not isolated events for most people (Corr & Corr, 2020; Tyrrell et al., 2023). Figure 2 provides further insight into each stage's underlying emotions and concepts.
Figure 2
Kübler-Ross Grief Cycle

Signs of Grief
The signs and symptoms of grief vary widely interpersonally and intrapersonally. In addition to those highlighted in Figure 2, grief can manifest across a spectrum of emotions, feelings, physical sensations, and behaviors. People who are grieving experience sadness and sorrow commonly, which may or may not be expressed by crying. Feelings of disbelief, helplessness, numbness, and shock are common. These feelings primarily serve as defense mechanisms to safeguard the bereaved from feeling overwhelmed by the pain of the loss. Guilt is common and may be related to 'survivor's guilt, unfinished business, or grounded in irrational thoughts that the death could have somehow been prevented. Some people may feel emotionally isolated and detached from others, whereas others may intentionally detach from others to protect themselves from being hurt by the loss of another person. Grief's most common physical manifestations include fatigue, exhaustion, insomnia, headaches, joint pain, dry mouth, muscle aches, and gastrointestinal ulcers. Anxiety is one of the most common emotions experienced following the death of a loved one. It is often accompanied by nausea, anorexia, chest tightness, irritability, and restlessness. Cognitive manifestations can include excessive worry, fear, feelings of impending doom, an inability to concentrate, and a sense of confusion. People may become preoccupied with the deceased, and some describe hallucinations. Behavioral symptoms can involve withdrawal in the form of emotional or physical detachment from others. Performance at work or school may become impaired, and the bereaved may avoid any setting, situation, or circumstance that reminds them of the deceased (Mughal et al., 2022; NCI, 2022; Worden, 2018).
Types of Grief
There are several types of grief responses; some are considered normal and indicative of healthy grieving, whereas others suggest maladaptive coping with loss. The most common types of grief are described in this section.
Normal (Uncomplicated) Grief
Normal grief is considered the most desirable and universal reaction to loss. Approximately 50% to 85% of individuals experience normal or uncomplicated grief. This type of grief often includes a variety of signs and symptoms from the physical, emotional, cognitive, or behavioral domains of loss. Normal grieving generally centers on the decrease of grief-related symptoms and the gradual movement toward acceptance of the loss, as the bereaved eventually adjust to the loss and move forward with life. While there is no finite period that one is expected to navigate through the stages of grief, there is a gradual movement toward growth and healing in a typical grief experience. The duration of uncomplicated grief varies from person to person and is dependent on individual factors related to the circumstances surrounding the loss and the relationship of the bereaved with the deceased; however, the typical length of grieving is six months to two years (NCI, 2022; Oates & Maani-Fogelman, 2022; Wittkowski & Scheuchenpflug, 2021).
In 2022, the most recent version of the Diagnostic and Statistical Manual of Mental Disorders Text Revision (DSM-5-TR) added prolonged grief disorder as a diagnosis for those individuals that experience extended maladaptive grieving. It is estimated that 7% to 10% of adults and 5% to 10% of adolescents and children will meet the criteria of prolonged grief disorder following a loss. The development and inclusion of this disorder has been criticized due to the listed diagnostic criteria not considering the differences in usual grieving symptoms and length among individuals (American Psychiatric Association [APA], 2022a, 2022b). Table 1 outlines the specific aspects of normal grieving in direct comparison to the clinical features of prolonged grief disorder.
Table 1
DSM-5-TR Comparison of Normal Grieving and Prolonged Grief Disorder
Normal Grieving | Prolonged Grief Disorder |
Painful feelings come in waves, lessen in intensity and frequency over time, and are intermingled with positive memories of the deceased person. | Symptoms persist for at least 12 months after the individual has passed. |
The predominant effect includes emptiness and loss accompanied by occasional pleasant emotions. Thoughts or reminders of the deceased generally trigger a depressed mood. | The individual believes that a piece of themselves has died with the patient; is unable to believe that the death is real; avoids places and situations that remind them of the deceased; experiences intense emotions such as anger or bitterness; inability to reintegrate into society; loss of meaning in life; an intense feeling of loneliness. |
Self-esteem is usually preserved. | An inability to function in school or the workplace profoundly impacting social and family relationships. |
Thoughts of death and dying are usually focused on the deceased, reuniting with the deceased in death, or feelings of guilt toward specific gaps or failures in the relationship with the deceased. | An intense yearning or longing for the deceased person or a preoccupation with memories of the individual are present every day for at least a month. |
The individual maintains connections with family and friends, particularly those who can console the bereaved person. | The individual withdraws from others physically and emotionally and has difficulty being consoled by anyone. |
The individual is preoccupied with thoughts and memories of the deceased but tends to remain hopeful. | The individual is preoccupied with self-critical or pessimistic thoughts and tends to be hopeless. |
(APA, 2022a; Wittkowski & Scheuchenpflug, 2021)
Anticipatory Grief
Anticipatory grief is a response to an expected death and can start at the time of diagnosis and continue until the person dies. Anticipatory grief includes many of the same symptoms of normal grieving following death, but the distinction is that the ill person is still alive and present when the grieving begins. Anticipatory grief can be experienced by a loved one or the person expected to die. It is commonly experienced by family members of loved ones diagnosed with a chronic or terminal illness who grieve while the patient is alive due to the awareness of an impending loss. Dying patients can also experience anticipatory grief, foreseeing the loss of function, independence, or future absence from major live events, such as their children's marriage or their grandchildren's birth. This can be highly distressing to patients and accompanied by anxiety, fear, and heightened perceived pain levels (DeSpelder et al., 2020; Lowey, 2015). Not all patients with a terminal illness will experience anticipatory grief. According to the NCI (2022), approximately 25% of patients with incurable cancer experienced anticipatory grief. Anticipatory grief is more likely to occur in people with dependent relationships, limited social support, lower levels of education, neuroticism, and those facing spiritual crises. Conversely, anticipatory grief is less likely to occur when death is accepted by the patient and the 'patient's social network. Research has demonstrated that anticipatory grief may serve a vital and beneficial purpose for families and loved ones. It has been shown to reduce the negative impact of the bereavement period after death; patients and families who experience anticipatory grief and can accept death as an impending event endure less anxiety and depression and reacclimate to life following death with less difficulty (Lowey, 2015; NCI, 2022).
Complicated Grief
Complicated grief is precisely as it sounds: more complex and challenging to navigate and potentially requiring professional help to overcome depending on its severity. The feelings of loss are debilitating and do not improve over time, as expected with normal grief. Instead, the bereaved person has significant trouble recovering from the loss and resuming their life. Complicated grief is often characterized by anger and bitterness, recurrent painful emotions, and an inability to face death as a reality. The bereaved are often preoccupied with thoughts of the deceased, unable to focus on anything other than the loss, experience distressing or intrusive thoughts related to the death, and an intense yearning and longing for the deceased. The bereaved may lose the meaning associated with their life and a sense of purpose, making it difficult to carry out normal daily activities (Oates & Maani-Fogelman, 2022). Complicated grief consists of four subtypes or patterns, outlined in Table 2
Table 2
Four Patterns of Complicated Grief
Pattern | Description |
Chronic | Normal grief that continues for an extended or prolonged period |
Delayed | Normal grief reactions are suppressed or postponed (consciously or unconsciously) to avoid the pain. Symptoms of grief occur at a much later time than is typical. |
Exaggerated or Distorted | An intense reaction to loss that can include thoughts of suicide, phobias, or night terrors; a pattern characterized by extreme or atypical symptoms. |
Masked, Absent, or Inhibited | The affected individual is unaware that their behaviors are due to the loss and shows little evidence of the expected separation distress or other characteristics of normal grief. |
(Lowey, 2015; NCI, 2022)
Certain situations and factors can increase the risk of an individual experiencing complicated grief (DeSpelder et al., 2020). Examples include:
- enduring repeated loss or deaths that are sudden, traumatic, violent, or random, such as fatal accidents, homicide, or suicide
- a death that is drawn out due to a long-term illness
- the death of a child
- believing that the death was preventable
- presence of a mental illness
- a relationship between the deceased and bereaved that is dependent or ambivalent (DeSpelder et al., 2020)
Additional risk factors for complicated grief include a lack of social support, 'survivors' age younger than 60, lower income, a history of depression, and concurrent life stressors (DeSpelder et al., 2020; NCI, 2022).
Unresolved Grief
Unresolved grief occurs due to failure to move through the stages of grief and come to terms with the loss. Many theorists consider unresolved grief a component of complicated grief, as it shares many similar features to those described above. Unresolved grief lasts much longer than normal grief, does not improve with time, and interferes with the ability to function in daily life. It is usually associated with a lack of formal closure, such as if the loved 'one's body was never found or laid to rest or due to multiple or concurrent losses, such as losing several family members in a fatal accident. Bylund-Grenklo and colleagues (2016) explored the consequences of unresolved grief by conducting a nationwide population-based study of youth who lost a parent to cancer during their teenage years. They discovered that those with unresolved grief endure significantly more depressive symptoms, negative intrusive thoughts, fatigue, and sleep disturbances (Bylund-Grenklo et al., 2016).
Disenfranchised Grief
Disenfranchised grief is also called hidden grief, as it describes a loss that is not validated, openly acknowledged, publicly mourned, or socially supported. This type of grief commonly occurs in people who have lost loved ones to stigmatized illnesses such as AIDS or mental health disorders or through socially unacceptable or controversial modalities such as abortion or suicide. Disenfranchised grief can occur with the death of a partner in an unrecognized relationship, such as those in a same-sex relationship who have not yet revealed their sexual preference to their family and friends. It can also occur with miscarriage, stillbirth, the loss of a pet, or a previously severed relationship, such as with the death of an ex-spouse (Lowey, 2015; Luchterland, 2020).
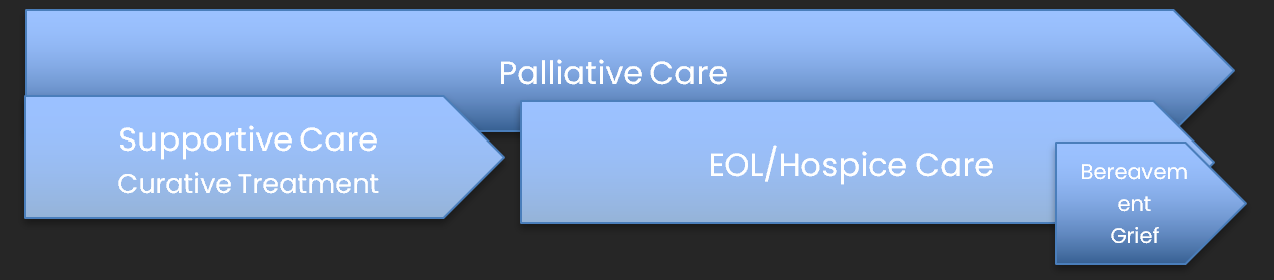
Nursing Grief and Loss
The nurse is a dedicated caregiver trained to provide physical, emotional, and psychological care to the patient and family. Nurses care for patients through all stages of their illness and treatment, which ultimately leads to the restoration of health or death of the patient. When death is possible, nurses strive to help patients and families empathetically come to terms with the impact of their illness, discuss wishes, set realistic care goals, and make appropriate EOL decisions (ANA, 2016). For nurses, each connection formed during this period will be accompanied by a subsequent loss once the patient dies. The toll and impact of this loss on the nurse can vary tremendously and is primarily grounded in the 'nurse's unique perspectives on death, beliefs, values, prior experiences with death, and several nursing-related factors. Some of the most prominent nursing-related factors that contribute to the grief response in nurses include the clinical practice subspecialty, the amount of exposure to patient death and dying in the workplace, the perceived comfort and skillset providing care for patients and communicating with families at the EOL, and how the death ensues. Oncology, palliative, and hospice nurses are exposed to death and dying much more frequently than nurses in other specialties (e.g., orthopedics or labor and delivery). Therefore, experienced oncology, palliative, and hospice nurses are often at greater ease communicating with patients and families about their care goals, including EOL care, advanced directives, and managing expectations surrounding the dying process. ICU and emergency room (ER) nurses are exposed to death in a manner that is dramatically different from those nurses practicing in oncology or hospice settings, as death may ensue rapidly and without notice. Families may be unprepared, and death is often more traumatic if the care goals are not discussed beforehand. Further, evidence demonstrates that the details surrounding the death experience (i.e., traumatic with several life-prolonging interventions versus an expected death with comfort care measures) can directly impact the 'nurse's emotional response and subsequent grieving process (Al-Majid et al., 2018).
How Grief Can Manifest in Nurses
Regardless of the practice setting, when a patient dies, the nurse may experience overwhelming emotion and grief; however, it is often ignored and suppressed. Unresolved or disenfranchised grief is widespread among nurses, as they usually do not have the time or capacity to mourn the loss of a patient before moving on to care for the next patient. Research has demonstrated that nurses consciously and subconsciously develop strategies to avoid grieving the death of a patient, allowing them to continue providing supportive nursing care to other patients. Nurses often continue working despite their grief as they serve as the support system for bereaved families in the immediate post-death period. Suppressing feelings associated with the death of a patient can inflict a heavy burden that can accumulate over time. In addition to disallowing themselves time to grieve, nurses often deny themselves compassion. They hesitate to seek help due to the misguided understanding that a good nurse remains tough and develops "thick skin." Eventually, the compilation and burden of unresolved grief can manifest in a complex array of emotional, cognitive, psychological, and physical symptoms. In addition to the symptoms described earlier, nurses may experience intense physical and emotional exhaustion, high moral distress, lack of concentration, unhappiness, depersonalization, burnout, and compassion fatigue (Boerner et al., 2017; Tranter et al., 2016; Yilmaz, 2017).
Compassion fatigue is a broadly defined concept that is well-cited in nursing, as up to 40% of nurses will experience it at some point in their careers. Compassion fatigue is characterized by the physical, emotional, and spiritual exhaustion and distress that results from caring for patients and long-term exposure to recurrent human suffering and death. It can manifest as many physical, emotional, spiritual, and psychological health ailments and induce interpersonal and psychosocial problems. Compassion fatigue is commonly associated with an inability to provide compassionate care or the depersonalization of care. This leads to a decline in the quality of patient care, job dissatisfaction, decreased morale, and burnout. Unaddressed emotional distress and grief can lead to reduced productivity in the workplace through increased absenteeism and increased staff turnover; this has a ripple effect on the remaining staff, who need to absorb the impact of fewer nurses. Further, these consequences fuel a rise in healthcare costs to the institution and society and contribute to the nursing shortage (Cross, 2019; Fallek et al., 2019; Gustafsson & Hemberg, 2022; Perregrini, 2019).
One of the consequences of compassion fatigue is moral distress. Moral distress encompasses the anxiety, tension, and behaviors that result from repeated loss and prolonged exposure to patient suffering, specifically in response to personal beliefs and values that conflict with the circumstances surrounding the 'patient's care. Ethical issues at the EOL are a significant source of moral distress among nurses; this includes the continued delivery of aggressive interventions to dying patients despite minimal or no clinical benefit, as well as decisions to withdraw care. These responsibilities can heighten stress and trigger feelings of powerlessness, hopelessness, and vulnerability (Boerner et al., 2017; Cross, 2019). For more information on this topic, please refer to the NursingCE course entitled Ethical Issues at the End of Life.
Emotionally exhausted caregivers may experience symptoms similar to post-traumatic stress disorder, such as recurrent recollections, distressing dreams, and anxiety. Unresolved grief in nurses is associated with reduced cognitive ability, medication errors, and impaired clinical judgment. Feelings of isolation, anger, and guilt can develop, in addition to a loss of self-worth and purpose. Some additional signs of declining physical and mental health may include behavioral changes and mood swings. These may be observed by peers or patients and communicated through complaints and dissatisfaction with the care they received. Nurses may appear lethargic, disinterested in patient care, delayed in response to patient needs, or neglecting responsibilities. They may become more vocal about job dissatisfaction, complain about patient assignments, or disengage in unit-based activities and committees. These changes can also affect 'one's personal life as acknowledged by family and friends and present as increased conflict, arguing, and irritability with close contacts, or by disinterest, withdrawal, or not spending time with loved ones. Dietary and physical activity patterns may change, such as a lack of desire to exercise, weight gain, and overall neglect of personal health. In extreme cases, nurses may develop addictive behaviors, such as diverting or abusing drugs or alcohol (Fallek et al., 2019; Perregrini, 2019).
The nursing environment, expectations surrounding death, and the type of death also contribute to the severity of the 'nurse's grief. Certain nursing specialties (e.g., oncology, hospice, palliative, dialysis) care for patients for an extended period through the continuum of their disease process. There is abundant literature dedicated to grieving patient loss among dialysis and oncology nurses, who regularly care for patients over weeks, months, or even years. Over time, caring relationships are fostered by nurses, generating strong emotional bonds and attachments between the nurse and the patient and family. Ultimately, this can make the patient's death feel like a personal loss to the nurse. Repeated encounters with patients that are suffering or dying can make grieving more complex and remind nurses of their mortality or the mortality of their loved ones. Several sources cite that it has been perceived as taboo to grieve the loss of a patient in an ICU setting due to the relatively short duration of these caregiving relationships. However, when patient outcomes are less than expected, it can lead to a loss of self-image or professional identity for the nurse (Al-Majid et al., 2018; Cross, 2019; Luchterland, 2019).
Grieving Bad Deaths
The term good death emerged in the US and Europe in the 1960s and was primarily used as a synonym for euthanasia, where life was deliberately put to an end. It became a key concept during the hospice and palliative care movement. Today, nurses and other direct healthcare professionals view death as good when it is physically comfortable, emotionally and spiritually healthy, and centered on respect and dignity. The patient and family are aware and prepared for the approaching death and perceive their needs as met. The patient receives interventions per their wishes and is surrounded by loved ones in a peaceful environment. Conversely, bad deaths are characterized by physical suffering, social isolation, psychological and emotional anguish, and care that may be discordant with the 'patient's and 'family's preferences. Bad deaths are more difficult to grieve, as they destroy the expectation and vision of an ideal and peaceful death. Bad deaths can preclude loved ones from having meaningful conversations, resolving unfinished business, or receiving closure. Nurses who witness bad deaths observe human suffering and pain on disturbing levels; they may internalize these traumatic experiences, fueling their fears of death, dying, and suffering (Carr et al., 2020; Krikorian et al., 2020).
Strategies for Coping with Death and Grief
Unaddressed grief has severe consequences and is more complex for nurses who lack the proper skill set, training, knowledge, attitudes, and support system to facilitate healthy coping. Nurses who lack the coping skills to effectively manage patient death may be inadequate in supporting dying patients and their family members. Nurses who recognize and confront their feelings and reactions to death can develop healthier coping skills and provide higher-quality care and support to their patients. In addition, nurses who allow themselves to go through the grieving process are healthier overall and lead more fulfilling lives and careers. Alternatively, those who do not allow themselves to grieve eventually struggle with sustaining satisfying careers and positive relationships. These nurses may also lose their self-confidence and feel a sense of guilt over losing a patient. They also tend to become more distant and are more reluctant to get close to their patients (Houck, 2014; Kostka et al., 2021; Zheng et al., 2018)
A critical step in preventing the potential negative consequences of unresolved grief is recognition. Nurses need to take the time to acknowledge each 'patient's death. Nurses are better positioned to make more positive judgments about navigating through grief by developing insight into and awareness of their personal feelings surrounding death. Nurses are encouraged to acquire a heightened awareness and understanding of their personal beliefs and values surrounding death and their preexisting coping strategies, both the good and the bad. These mindfulness activities can help nurses develop more positive and effective coping skills and ensure that personal beliefs do not negatively impact or influence patient care. The fundamental aspects of coping with patient death include self-care, work-life balance, communication skills, a social support network, and emotional resiliency. Ideally, this should begin in nursing school so the new graduate nurse is prepared and equipped with strategies to preserve their health and well-being before entering the workplace (Houck, 2014).
Self-Care
Self-care is a core value of holistic nursing and is a proactive and personalized approach to fostering well-being. It refers to any activity one engages in to promote overall health. Nurses who care for themselves grieve better, endure significantly fewer negative consequences of grief, and have an enhanced capacity to provide compassionate care to patients and families. Nurses must recognize that effective self-care is a continually evolving work-in-progress that should remain a priority in both personal and professional environments (Mills et al., 2018). There are countless ways nurses can engage in self-care, but some of the most well-cited strategies include the following:
- take breaks and time to disconnect periodically, especially during long shifts
- engage in healthy lifestyle choices and behaviors, including adequate sleep, rest, hydration, exercise, and healthy eating habits
- identify ways to rejuvenate well-being, such as through music, yoga, relaxation therapies (mindfulness, meditation, reiki, hot bath, massage)
- engage in enjoyable activities as desired (reading, gardening, socializing, etc.)
- seek support from colleagues, friends, or loved ones
- make time for spiritual or religious practices such as praying, attending religious services, or retreats
- develop an appropriate work-life balance by establishing and maintaining boundaries within and outside of the workplace:
- invest in meaningful relationships with friends and family
- allow space for non-nursing activities
- take dedicated time away from work
- shed the professional role after the workday
- build and maintain positive and healthy interpersonal relationships within the professional environment and personal life
- manage personal life stressors (Houck, 2014; Gibson et al., 2018; Mills et al., 2018; Perregrini, 2019)
Communication and Social Support
Nurses need to identify social support networks and lean on them when needed. Effective communication skills and social support are critical to fostering healthy grieving. Communication cultivates robust connections within the team. Adapting a workplace environment of 'sharing and caring,' with regular debriefing sessions, grief counseling sessions, and support from supervisors and colleagues, is a valuable grieving strategy. Nurses with access to supportive environments to effectively debrief following an arduous clinical experience are better positioned to maintain health and professionalism and are less likely to endure compassion fatigue. Bereavement literature consistently demonstrates that support and understanding from fellow nurse coworkers is a crucial way of effectively coping with loss (Gibson et al., 2018; Houck, 2014).
There is a three-step process to facilitate addressing the trauma that can result from caring for dying patients: defusing, debriefing, and follow-up. Defusing should occur on the same day as the event, followed by debriefing a few days later. Debriefing with nursing colleagues following a 'patient's death is one of the most effective tactics for processing difficult experiences. There are different phases of debriefing, including the description or reaction, analysis, and application or summary. Informal debriefing sessions are preferred over formalized ones, as they produce a higher level of intimacy among colleagues facing similar situations. These informal debriefing sessions allow for mutual support between colleagues, creating a safe environment for processing painful emotions and facilitating open discussion of the distressing events surrounding the loss. These sessions have been shown to foster emotional growth and aptitude among nurses. Informal debriefing with coworkers is preferred over support from family and loved ones. Nurses perceive debriefing with coworkers as more validating, effective, and cathartic than support from significant others or spouses. Many feel their loved ones often cannot fully comprehend or understand their experiences and cannot provide sufficient acknowledgment or validation of their loss. In addition, some nurses find it therapeutic to grieve with the family through crying, prayer, or attending the patient's funeral or memorial services. Follow-up should occur to ensure that the nurse is coping effectively and suggest professional help if needed (DeSpelder et al., 2020; Edwards et al., 2021; Knott et al., 2023).
Emotional Resiliency
Emotional resiliency is at the core of coping with death and grief and is an important protective factor against compassion fatigue, emotional exhaustion, burnout, and disenfranchised grief in nurses. Resilience is an individual's ability to overcome or adapt to complicated circumstances and function in a challenging environment while preserving health and well-being and fostering personal growth. It refers to the individual's capacity to respond to the pressure and demands of daily life and is a survival skill. Some people are innately more resilient than others, and some develop resiliency over time through hardship and life experiences. Factors that promote resiliency include positive social relationships, hope, optimism, spirituality, organizational support, self-efficacy, and having a resilient role model. By maintaining emotional resiliency, nurses are better equipped to provide the best care for themselves and others experiencing grief. Moral distress is a significant predictor of nursing burnout, as there is a strong association between burnout and those with low levels of resilience. A higher level of resiliency protects nurses from emotional exhaustion and is associated with increased hope and reduced stress, burnout, and compassion fatigue and contributes to heightened personal accomplishment. Correspondingly, nurses with low emotional resilience experience more compassion fatigue and job dissatisfaction (Andersen et al., 2021; Oates & Maani-Fogelman, 2022; Yilmaz, 2017).
Self-care factors such as work-life balance, control, maintaining hope, a sense of professional identity, and perceived emotional support contribute to 'nurses' resilience. Higher resilience levels are linked to enhanced self-efficacy, coping, and competence. The ability to cope effectively with pressure, trauma, and uncertainty is premised on underlying behaviors, thoughts, and actions. Many strategies that promote emotional resiliency are also firmly grounded in self-care principles (Yilmaz, 2017). Some of the most effective ways to build emotional resiliency include the following:
- cognitive restructuring centered on generating optimism and positive attitudes
- psychotherapy to resolve underlying anxieties, fears, or unresolved issues
- journaling or blogging
- exercising, yoga, meditation, or mindfulness
- spirituality and religious beliefs
- shifting mental focus toward the things that are within the 'nurse's locus of control and away from the things that are not
- improving self-confidence as a person and as a nurse
- leaning on social networks for support (colleagues, spouse, family, friends)
- engaging in open communication in the workplace and within the 'nurse's personal life to maintain more fulfilling relationships
- anything that promotes or facilitates the development of inner strength that can be used to maintain health and well-being (Yilmaz, 2017)
Although nurses need to take responsibility for developing effective personal strategies to manage grief and facilitate successful coping and emotional resiliency, organizational support is also an integral element in helping nurses cope with loss. Unfortunately, loss and bereavement remain insufficiently addressed across healthcare settings. One literature review revealed a lack of emotional support and resources consistently available to nurses when patients die, even in the oncology and hospice fields, where death is commonplace. Lack of employer support in acknowledging and dealing with patient loss, grief, and bereavement is a recurrent theme across the literature. Many interventions listed in the literature are employee-driven and not initiated by the employer. Healthcare administrators and nurse leaders are fundamental to the early identification of nurses at risk for compassion fatigue and complicated grief. Developing and implementing bereavement programs designed explicitly for nurses can provide the time, environment, and skills training to channel emotions surrounding patient death in a healthy manner. Leaders can reduce burnout, turnover, and compassion fatigue and enhance job satisfaction by generating a supportive environment and educating on recognizing and adequately managing personal bereavement (Gibson et al., 2018; Perregrini, 2019; Soper, 2022). Strategies proposed in the literature include the following:
- monthly grief rounds
- facilitated discussion groups, offering outlets for sharing emotional expressions, remembrance ceremonies, debriefings, retreats, professional counseling, and pastoral care services
- staff training through a bereavement care service or other programs, providing education and training to develop behaviors that aid in coping, effective communication, and healthy ways of working through grief and loss
- group processing through writing, storytelling, journaling, memory boards, or books
- skills training to build resilience, compassion, and effective self-care practices
- interventions centered on creating a more supportive work environment, ensuring adequate nursing breaks and time off, and adjusting patient care assignments (Boerner et al., 2017; Fallek et al., 2019; Houck, 2014; Perregrini, 2019)
References
Al-Majid, S., Carlson, N., Kiyohara, M., Faith, M., & Rakovski, C. (2018). Assessing the degree of compassion satisfaction and compassion fatigue among critical care, oncology, and charge nurses. The Journal of Nursing Administration, 48(6), 310-315. https://doi.org/10.1097/NNA.0000000000000620
American Nurses Association. (2016). Nurses' roles and responsibilities in providing care and support at the end of life. https://www.nursingworld.org/~4af078/globalassets/docs/ana/ethics/endoflife-positionstatement.pdf
American Psychiatric Association. (2022a). Diagnostic and statistical manual of mental disorders: DSM-5-TR (5th ed.). American Psychiatric Association.
American Psychiatric Association. (2022b). Prolonged grief disorder. https://www.psychiatry.org/patients-families/prolonged-grief-disorder
Andersen, S., Mintz-Binder, R., Sweatt, L., & Song, H. (2021). Building nurse resilience in the workplace. Applied Nursing Research, 59 (51433). https://doi.org/10.1016/j.apnr.2021.151433
Boerner, K., Gleason, H., & Jopp, D. S. (2017). Burnout after patient death: Challenges for direct care workers. Journal of Pain and Symptom Management, 54(3), 317-325. https://doi.org/10.1016/j.jpainsymman.2017.06.006
Bylund-Grenklo, T., Fürst, C. J., Nyberg, T., Steineck, G., & Kreicbergs, U. (2016). Unresolved grief and its consequences. A nationwide follow-up of teenage loss of a parent to cancer 6-9 years earlier. Supportive Care in Cancer, 24(7), 3095-3103. https://doi.org/10.1007/s00520-016-3118-1
Carr, D., Boerner, K., & Moorman, S. (2020). Bereavement in the time of coronavirus: Unprecedented challenges demand novel interventions. Journal of Aging & Social Policy, 32(4-5), 425-431. https://doi.org/10.1080/08959420.2020.1764320
Center to Advance Palliative Care. (n.d.). About palliative care. Retrieved July 14, 2023, from https://www.capc.org/about/palliative-care
Corr, D. M., & Corr, C. A. (2020). Elisabeth Kübler-Ross and the 5 Stages Model in a sampling of recent North American nursing textbooks. Journal of Hospice & Palliative Nursing, 22(1), 61-67. https://doi.org/10.1097/NJH.0000000000000615
Cross, L. A. (2019). Compassion fatigue in palliative care nursing: A concept analysis. Journal of Hospice & Palliative Nursing, 21(1), 21-28. https://doi.org/10.1097/NJH.0000000000000477
DeSpelder, L. A., Stickland, A. L., Potts, J. M., & Mason, M. (2020). The last dance: Encountering death and dying (11th ed.). McGraw Hill.
Edwards, J. J., Wexner, S., & Nichols, A. (2021). Debriefing for clinical learning. Agency for Healthcare Research and Quality. https://psnet.ahrq.gov/primer/debriefing-clinical-learning
Fallek, R., Tattelman, E., Browne, T., Kaplan, R., & Selwyn, P. A. (2019). Original research: Helping health care providers and staff process grief through a hospital-based program. American Journal of Nursing, 119(7), 24-33. https://doi.org/10.1097/01.NAJ.0000569332.42906.e7
Freud, S. (1917). Mourning and melancholia. Metapsychology, IV, 152-170. http://www.columbia.edu/itc/hs/medical/clerkships/psych/misc/articles/freud.pdf
Gibson, K., Hofmeyer, A., & Warland, J. (2018). Nurses providing end-of-life care for infants and their families in the NICU: A review of the literature. Ethical Issues in Neonatal Care, 18(6), 471-479. https://doi.org/10.1097/ANC.0000000000000533
Gustafsson, T., & Hemberg, J. (2022). Compassion fatigue as bruises in the soul: A qualitative study on nurses. Nursing Ethics, 29(1), 157-170. https://doi.org/10.1177/09697330211003215
Houck, D. (2014). Helping nurses cope with grief and compassion fatigue: An educational intervention. Clinical Journal of Oncology Nursing, 18(4), 454-458. https://doi.org/10.1188/14.CJON.454-458
Knott, H., Dambrino, K. L., Busby, S., & Rasmussen, A. (2023). Debriefing among hospice professionals during a pandemic. Journal of Hospice & Palliative Nursing, 25(2), 90-96. https://doi.org/10.1097/NJH.0000000000000930
Kostka, A. M., Borodzicz, A., & Krzeminska, S. A. (2021). Feelings and emotions of nurses related to dying and death of patients - A pilot study. Psychology Research and Behavior Management, 14, 705-717. https://doi.org/10.2147/PRBM.S311996
Krikorian, A., Maldonado, C., & Pastrana, T. (2020). Patient's perspectives on the notion of a good death: A systematic review of the literature. Journal of Pain and Symptom Management, 59(1), 152-164. https://doi.org/10.1016/j.jpainsymman.2019.07.033
Lowey, S. E. (2015). Nursing care at the end of life: What every clinician should know. OPEN SUNY Textbooks. https://milnepublishing.geneseo.edu/nursingcare
Luchterland, C. (2020). Health care professional as griever: The importance of self-care clinical tool. https://www.va.gov/WHOLEHEALTHLIBRARY/tools/health-care-professional-as-griever-the-importance-of-self-care.asp
Mills, J., Wand, T., & Fraser, J. A. (2018). Exploring the meaning and practice of self-care among palliative care nurses and doctors: A qualitative study. BMC Palliative Care, 17(63). https:/doi.org/10.1186/s12904-018-0318-0
Mughal, S., Azhar, Y., Mahon, M. M., & Siddiqui, W. J. (2022). Grief reaction. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK507832
National Cancer Institute. (n.d.). End-of-life care. Retrieved July 14, 2023, from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/end-of-life-care
National Cancer Institute. (2022). Grief, bereavement, and coping with loss (PDQ®)–Health professional version. https://www.ncbi.nlm.nih.gov/books/NBK66052
National Hospice and Palliative Care Organization. (n.d.). Hospice care overview for professionals. Retrieved July 14, 2023, from https://www.nhpco.org/hospice-care-overview
Oates, J. R., & Maani-Fogelman, P. A. (2022). Nursing grief and loss. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK518989
Perregrini, M. (2019). Combating compassion fatigue. Nursing2019, 49(2), 50-54. https://doi.org/10.1097/01.NURSE.0000552704.58125.fa
Soper, K. (2022). Reducing burnout and promoting professional development in the palliative care service. Journal of Hospice & Palliative Nursing, 24(3), 181-185. https://doi.org/10.1097/NJH.0000000000000847
Tranter, S., Josland, E., & Turner, K. (2016). Nurses' bereavement needs and attitudes towards patient death: A qualitative descriptive study of nurses in a dialysis unit. Journal of Renal Care, 42(2), 101-106. https://onlinelibrary.wiley.com/doi/epdf/10.1111/jorc.12147
Tyrrell, P., Harberger, S., Schoo, C., & Siddiqui, W. (2023). Kubler-Ross stages of dying and subsequent models of grief. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK507885
Wittkowski, J., & Scheuchenpflug, R. (2021). Evidence on the conceptual distinctness of normal grief from depression. European Journal of Health Psychology, 28(3), 101-110. https://doi.org/10.1027/2512-8442/a000077
Worden, J. W. (2018). Grief counseling and grief therapy: A handbook for the mental health practitioner (5th ed.). Springer Publishing Company, LLC.
World Health Organization. (2020). Palliative care. https://www.who.int/news-room/fact-sheets/detail/palliative-care
Yarbro, C. H., Wujcik, D., & Gobel, B. H. (2018). Cancer nursing: Principles and practice (8th ed.). Jones and Bartlett Publishers.
Yilmaz, E. B. (2017). Resilience as a strategy for struggling against challenges related to the nursing profession. Chinese Nursing Research, 4(1), 9-13. https://doi.org/10.1016/j.cnre.2017.03.004
Zheng, R., Lee, S. F., Bloomer, M. J. (2018). How nurses cope with patient death: A systematic review and qualitative meta-analysis. Journal of Clinical Nursing, 27(1-2), e39-e49. https://doi.org/10.1111/jocn.13975